One of the most exciting things about working at CCRM Fertility is that the field of fertility medicine, or reproductive endocrinology, is constantly evolving. Science and technology have come so far since the first IVF baby, Louise Joy Brown, was born in 1978, and CCRM has been at the forefront of so many technological advances in IVF treatment throughout our 35+ years in the industry.
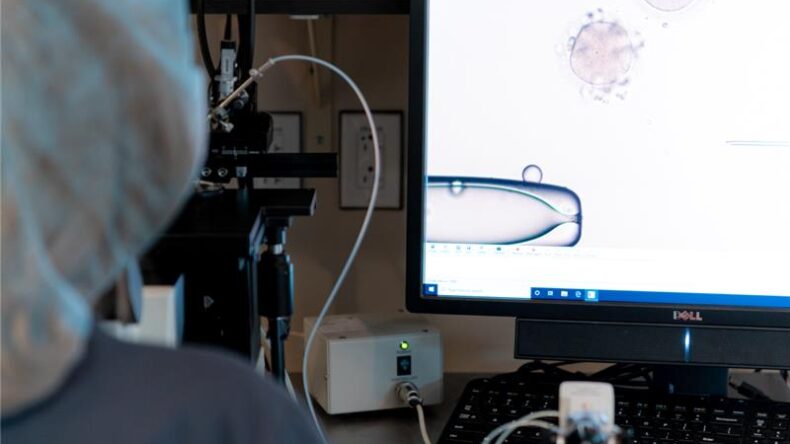
Among these incredible technologies is in vitro maturation, or IVM, a new procedure where immature oocytes are retrieved and then matured in an IVF lab. CCRM’s dedicated research and development team has been advancing IVM through extensive research, and the results from our IVM clinical trials are exciting and encouraging.
Here we explain what IVM is, how it can help treat infertility, and what you should know about CCRM’s IVM study for PCOS patients, which is currently in clinical trials.
What is IVM?
In vitro maturation involves retrieving immature oocytes from small follicles in the ovaries and maturing them in the IVF lab. There are two phases to the IVM process after the oocytes are retrieved:
- The oocytes are placed in a special pre-IVM media designed to take all the oocytes and synchronize their maturity to minimize heterogeneity. Think of the pre-IVM media like the holding pen for runners at a marathon.
- The synchronized oocytes are matured in the IVM media with hormones overnight, and by the next afternoon, the mature eggs are ready to be fertilized in the lab via intracytoplasmic sperm injection (ICSI).
What’s the difference between IVM and IVF?
The main difference between IVM and IVF is that in IVM, the immature oocytes are retrieved from small follicles with no or minimal hormonal stimulation. In conventional IVF, the mature oocytes are retrieved from large follicles with high doses of hormonal stimulation.
Another difference is that in an IVF cycle, the trigger shot is given about 36 hours before oocyte retrieval to initiate the final maturation of the oocytes within the body. In IVM, there is no trigger shot, because the oocytes are retrieved from the ovaries before they reach maturity.
Once the oocytes are mature, the process aligns with conventional IVF: mature oocytes are fertilized in the lab with sperm and watched closely to see which fertilized oocytes develop into blastocysts. A blastocyst is later transferred into the uterus to attempt pregnancy.
IVM for PCOS
Polycystic ovarian syndrome (PCOS) can cause infertility because people with this condition do not ovulate, or release an oocyte, due to a hormone imbalance. The ovaries fail to respond to the brain’s signal to grow and ovulate an oocyte, so, instead of getting released each month during the menstrual cycle, the oocytes ‘collect’ and build up in the follicles.
Patients with PCOS often have elevated anti-Müllerian hormone (AMH) levels, reflecting a higher number of antral follicles and immature oocytes. However, the hormonal imbalance in PCOS can impair oocyte development, leading to reduced quality. IVM may benefit these patients by retrieving and maturing these oocytes in the laboratory, which can increase the chances of obtaining high-quality oocytes for fertilization and development into viable embryos.
Other benefits of IVM for PCOS
Patients with PCOS are at increased risk of developing ovarian hyperstimulation syndrome (OHSS) because their high follicle count increases the likelihood of an exaggerated response to stimulation medications such as Gonal-F and Menopur.
IVM requires much fewer hormone injections and virtually eliminates the risk of OHSS (as well as all the accompanying side effects of the stim meds).
CCRM’s IVM study for PCOS
CCRM’s research and development team has been conducting 10 years of research in clinical trials for IVM with patients of varying diagnoses, including high body mass index (BMI) or diminished ovarian reserve (DOR). In two of our previous IVM studies, initial results found that 41% of PCOS patients who had received IVM treatment have had live births or an ongoing pregnancy.
CCRM is now conducting an IVM clinical trial and study exclusively for patients with PCOS and/or for women who meet the following criteria:
- 18-38 years old
- BMI <35
- PCOS diagnosis or good ovarian reserve with an AMH of >3.5 and antral follicle count (AFC) of >25
As of 2025, CCRM is enrolling 50 patients total and currently has less than 15 spots remaining.
Since the first oocyte retrieval in late 2023, our clinical trial has already demonstrated remarkable outcomes, including 15 embryo transfers plus five live births and counting.
What is the IVM process?
In CCRM’s IVM study, participants undergo just three days of ovarian stimulation before the oocyte retrieval on day 5.
The IVM process typically looks like this:
- Before the cycle: CCRM’s One Day Work-up followed by birth control pills to sync the menstrual cycle
- Day 1: Baseline ultrasound and blood draw
- Day 2-4: Stimulation; 150 ius of FSH, follicle-stimulating hormone, such as Gonal-F
- Day 5: Oocyte retrieval
How can I enroll my patients in the CCRM IVM clinical study?
If your patient may meet the criteria above and wants to be involved, please have them email researchstudy@ccrmivf.com to complete the study questionnaire and send any applicable records to the team.
Participants in the study get:
- free fertility workup
- free IVM cycle
- free preimplantation genetic testing (PGT)
- free first frozen embryo transfer (FET)
Patients will be responsible for travel expenses to our flagship CCRM clinic in Lone Tree, CO, as well as some medications for the FET, ranging on average between $2,000 to $7,000.
Why choose CCRM for IVM?
CCRM is the only fertility clinic in the United States currently conducting research on and performing in vitro maturation without a trigger shot for qualified patients.
We have 35+ years of experience researching and innovating in our field and are proud to shape the future of fertility care and reproductive science. IVM is only getting started!
Want to learn more? Tell your patients to book their fertility consultation at CCRM today.